The advance healthcare directive is an essential document through which individuals can specify how they wish to be treated in certain medical situations. But under what circumstances does this document remain valid, and when might its validity be questioned?
In this article, we provide you with a comprehensive guide on the validity of advance healthcare directives. You'll find detailed information on the criteria that determine the effectiveness of a directive, special circumstances such as cognitive impairment or being in a medically induced coma, and the formal requirements that should be followed when drafting such a directive.
For basic explanations on advance healthcare directives, this article can serve as a foundation: What is an advance healthcare directive?
Requirements for the Effectiveness of an Advance Healthcare Directive
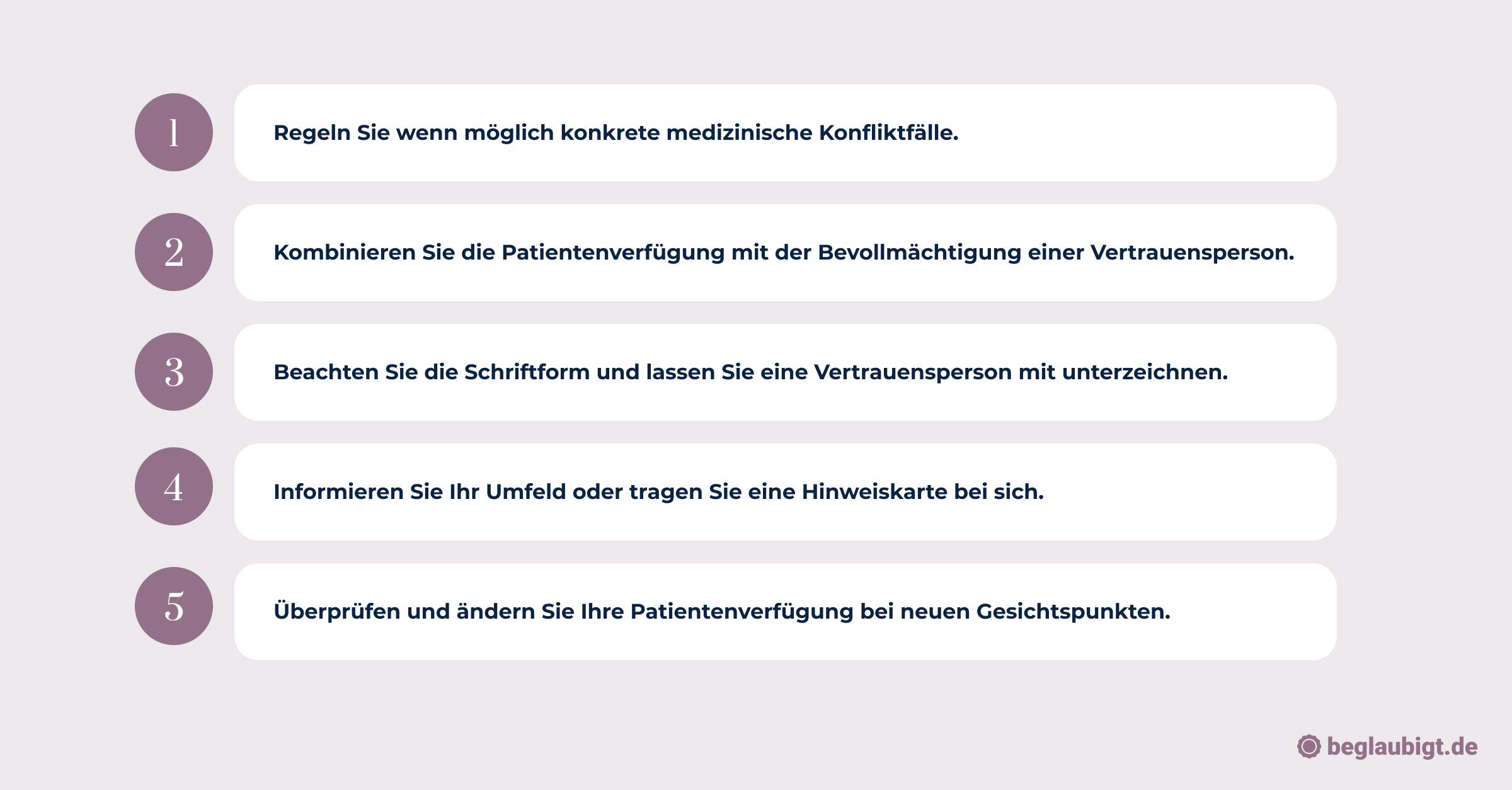
To be valid, an advance healthcare directive must meet certain requirements. Below is a summary of the key points:
- Written form and personal signature: A verbal declaration or mere expression of will is not sufficient. The directive must be in writing and personally signed by the author.
- Legal adulthood and decision-making capacity: The author must be of legal age and capable of understanding the consequences of their decisions at the time of drafting the directive.
- Clear wording: The directive should be clearly worded and include specific instructions for situations where the author is unable to make decisions.
- Regular review: The directive should be reviewed regularly and updated as necessary to ensure it reflects the author’s current wishes and preferences.
- Informing family and close persons: It is advisable to inform family and close individuals about the existence and contents of the directive to ensure clarity in an emergency.
- Durable power of attorney for healthcare: An advance healthcare directive can also be used in conjunction with a durable power of attorney for healthcare to ensure that the author’s wishes are respected, even when they are no longer able to make decisions themselves.

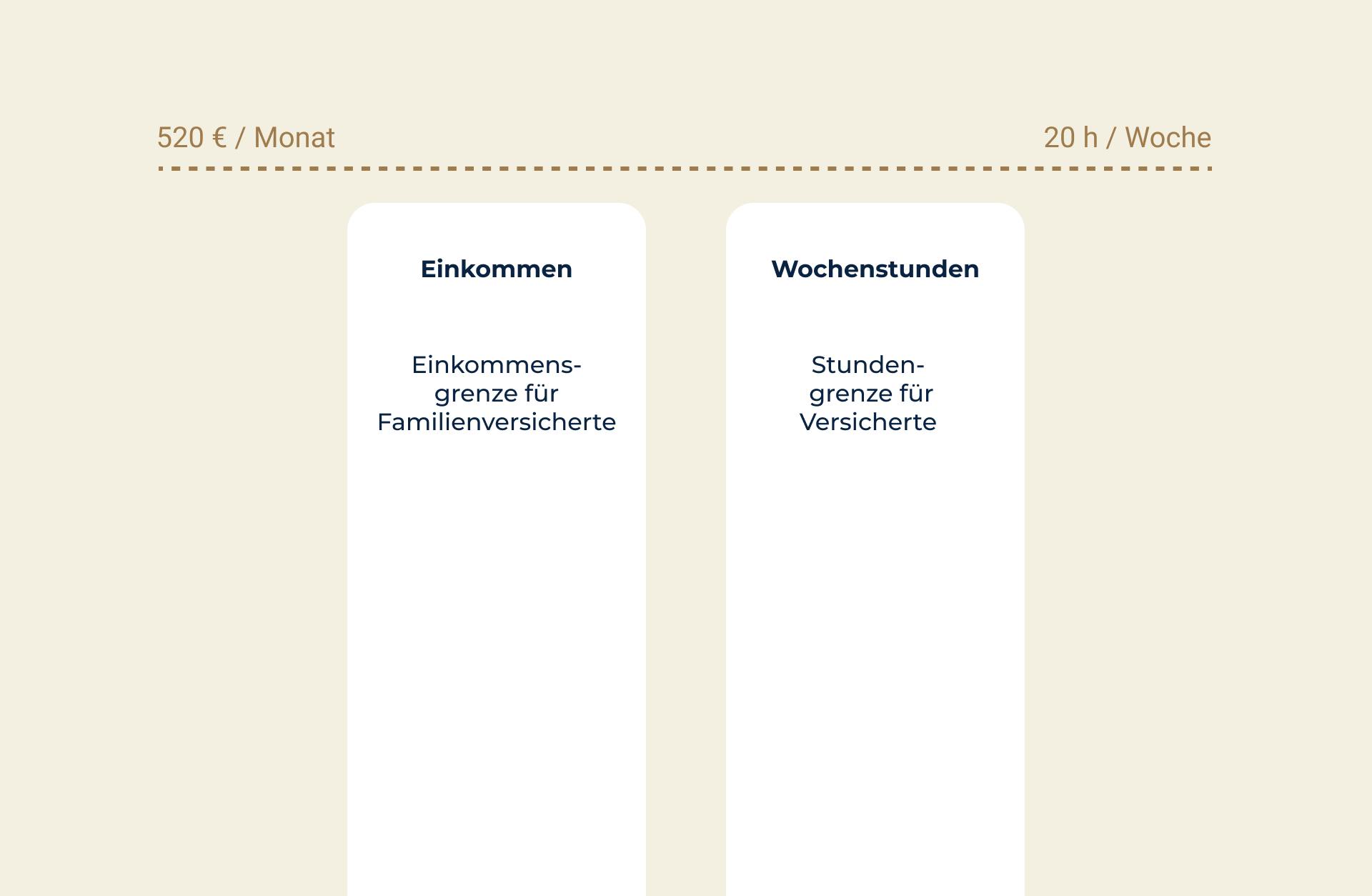
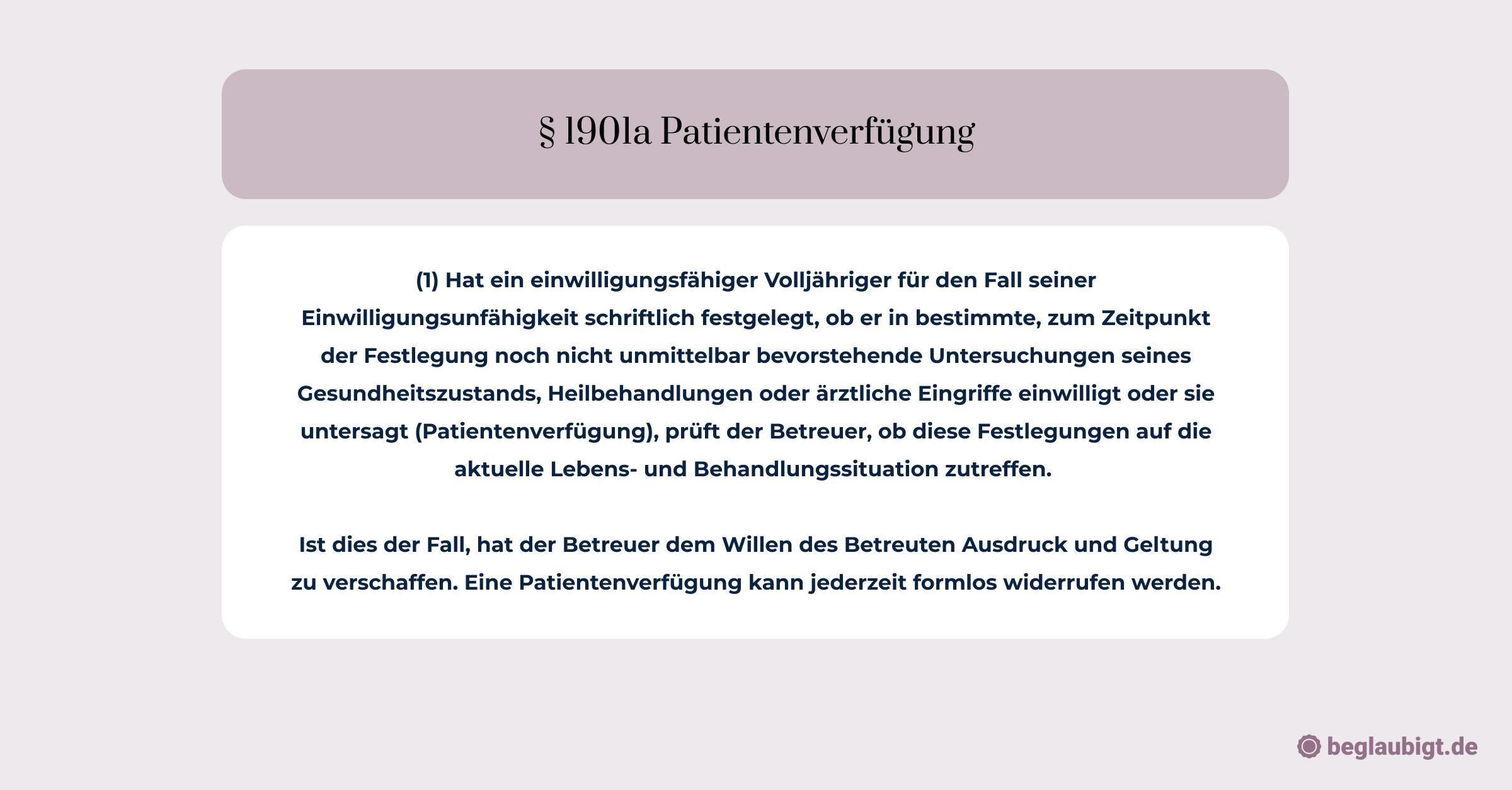
The requirements for the validity of an advance healthcare directive are indeed diverse and should be carefully observed to ensure a legally binding decision can be made in an emergency. These points are also anchored in various laws and regulations, such as the Advance Healthcare Directive Act (§ 2 Abs. 1) and the Civil Code (§ 1901a).
When Does an Advance Healthcare Directive Take Effect?
An advance healthcare directive generally comes into effect when the individual is no longer capable of making their own decisions. This can occur in cases of severe illness, disability, or advanced age. It is important that the person was capable of making decisions freely and understood the implications of those decisions at the time the directive was created.
Another requirement for the validity of an advance directive is that it must be clearly and specifically worded. It should be evident which medical treatments are desired or refused. Vague language or general statements may lead to interpretation difficulties in an emergency, hindering the implementation of the directive.
Additionally, the directive must be presented in its original form, signed by the individual. A copy or an electronic version is not sufficient. An advance directive can also be drafted by another person on behalf of the individual, but this person must be expressly authorized, and the directive must be signed in the presence of the individual.
It is advisable to review and update the directive regularly. Changes in personal or health circumstances may result in the original directive no longer reflecting the individual’s current wishes. Regular review and updates help ensure that the directive is carried out when needed.
Overall, it is crucial that an advance healthcare directive is clearly and specifically worded, exists in its original form, and is personally signed by the affected individual.
Additionally, the directive should be regularly reviewed and updated if necessary to ensure that it continues to reflect the individual’s current wishes and preferences. Only in this way can it be guaranteed that, in the event of an emergency, the individual’s desires regarding medical treatment will actually be carried out. (Counterexample: Who decides if there is no advance healthcare directive?)
How Long is an Advance Healthcare Directive Valid?
The duration of validity for an advance healthcare directive depends on several factors. There is no legal time limit for its validity. The directive remains valid as long as the decisions reflect the individual’s will and have not been revoked or altered.
However, it is important to note that an advance directive may become invalid if it no longer aligns with current medical standards. In such cases, doctors are not bound by decisions based on outdated instructions.
For instance, a term like "life-sustaining measures" might be unclear and subject to varying interpretations.
Experts recommend reviewing and updating an advance directive every two to three years to account for changes in personal values or medical advancements.
Key Points:
- No legal time limit for the directive’s validity.
- The directive remains valid as long as it reflects the individual's will and has not been revoked or altered.
- Outdated language may render the directive invalid.
- Regular review and updates are recommended every 2-3 years.
- Platform Suggestion: Beglaubigt.de provides services for issuing legally valid documents.
A Practical Example
A person drafts an advance healthcare directive at the age of 40, stating that in the event of an incurable disease, no life-prolonging measures should be taken. At the age of 60, the person is diagnosed with a severe cancer.
Since the decisions made in the advance healthcare directive still reflect the individual’s will and have not been revoked or altered, the directive remains valid and binding in this case.
How Long is an Advance Directive Valid with a Clear Health Condition?
When the person who created the advance directive is in a clear and healthy state, the directive is typically not applicable. An advance healthcare directive only becomes relevant when the author is no longer able to make independent decisions about their medical treatment due to a serious illness or injury.
In a clear state of health, the person can make their own decisions regarding medical care, so the need for an advance directive is unnecessary at that moment.
When a person is in a clear and healthy state, they can make their own decisions regarding medical care, which means there is no immediate need for an advance directive.
However, such a directive should be created when the person believes they might no longer be able to make independent decisions due to illness or injury. It is advisable to prepare early, as complications can arise in emergencies (see: Who decides if there is no advance directive).
Importantly, an advance directive remains valid even if the person recovers and regains the ability to make decisions. As long as the directive has not been revoked or altered, it remains binding and must be followed by healthcare professionals if the person again faces a situation where they are unable to make decisions.
How Often Should an Advance Healthcare Directive Be Updated?
An advance healthcare directive should be reviewed and, if necessary, updated regularly. There are several reasons that warrant a revision:
- Personal Changes
- Medical Advancements
- Legal Changes:
- Unclear Wording
Experts often recommend reviewing the directive every two to five years. Significant life changes may warrant an earlier review. After each revision, the updated version should be shared with relevant parties. Beglaubigt.de provides a tool that generates an advance directive in PDF and WORD format and stores it online (Advance Directive PDF).
Effect Upon Onset of a Specific Illness or Deterioration of Condition
The Federal Court of Justice (BGH) ruled on March 17, 2010 (Az: XII ZB 189/09) that an advance healthcare directive is no longer binding if the condition or health status of the affected person has changed in a way that was not anticipated in the directive. This occurs when the patient’s situation differs from what was described in the directive, making it no longer applicable.
For example, a directive might state that life-sustaining measures are to be refused if the person is terminally ill and in an irreversible condition. However, if the health of the person improves and there is a chance of recovery, the directive would no longer be in effect.
In such cases, the attending physicians must act based on the current situation and cannot rely on the advance directive.
This is why it is important for an advance healthcare directive to be as specific and precise as possible. Regular reviews and updates are also necessary to ensure its continued relevance even if the person's health condition changes.
Revisiting and Redrafting the Advance Healthcare Directive: How Beglaubigt.de Provides a Solution
It is crucial that an advance directive is not simply created and then forgotten. Regular review and, if necessary, redrafting are advisable, as health conditions and personal preferences may change over time.
However, it is also important that any review and redrafting of the advance directive occur while the person is in a clear mental state to ensure its validity is not compromised. The Beglaubigt.de online platform offers a practical solution to ensure the validity and availability of the advance directive.
With digital storage on the platform, the advance directive is accessible at any time and protected against loss. Additionally, the documents are stored in a secure and privacy-compliant environment on the platform, ensuring legal bindingness and confidentiality.
When Does an Advance Directive Become Invalid?
The validity of an advance directive can be questioned for several reasons:
- Medical Standards: An advance directive may lose its validity if it no longer aligns with current medical guidelines and standards. For instance, outdated or vague phrases like "life-extending measures" could create ambiguities. A well-known case before the Federal Court of Justice showed that an overly general advance directive may be considered non-binding.
- Change in Individual Will: An advance directive reflects the author’s wishes at a specific time. If the person changes their mind over time and the directive is not updated accordingly, it may lose its relevance and thus its validity.
- Revocation of the Advance Directive: The author has the right to revoke the advance directive at any time. An explicit revocation renders the directive invalid, and it loses its effect.
- Legal Requirements: In certain jurisdictions, such as Germany, advance directives must meet specific formal and substantive requirements to be legally binding. A directive that fails to meet these requirements can be declared invalid.
- Timeliness of the Directive: With the dynamic development in medicine and evolving personal beliefs, an advance directive should be regularly reviewed for its relevance. If it no longer reflects the current values or informed will of the author, its validity may be compromised.
How Can an Advance Directive Be Revoked?
Revoking an advance directive is generally straightforward, as most countries, including Germany, do not impose specific formal requirements for revocation. However, following a few steps can ensure the revocation is effective and recognized:
- Written Revocation: While many legal systems do not require a written form, it is advisable to revoke the directive in writing. This provides clear evidence that the directive has been revoked.
- Clarity: The revocation should be clear and unambiguous. A simple statement like "I hereby revoke my advance directive dated [date]" is typically sufficient.
- Destroy Original and Copies: To avoid confusion, you should destroy the original and all copies of the advance directive once it has been revoked.
- Notify Relevant Parties: Inform anyone who has a copy of your advance directive or is aware of its existence, including doctors, hospitals, family members, appointed representatives, or legal professionals.
- New Directive: If you wish to create a new advance directive, ensure it is clearly differentiated from the old one and may even explicitly refer to the revocation of the previous directive.
- Documentation: It can be helpful to document the revocation and destruction of the old advance directive to prevent future misunderstandings.
Important Jurisprudence and Laws Regarding the Validity of Advance Directives
The validity of advance directives is an important topic in patient law. There are numerous court rulings and laws that address this issue. Below are five important rulings and laws that regulate the validity of advance directives and are of significant practical importance.
- Advance Directive Act (Patientenverfügungsgesetz - PatVG): The PatVG regulates the conditions and effectiveness of advance directives in Germany. It defines, among other things, what content a valid advance directive must include and under what circumstances it comes into effect.
- Decision of the Federal Court of Justice from September 17, 2014 (Az. XII ZB 61/14): The Federal Court of Justice ruled that an advance directive is also valid if the patient does not explicitly prohibit treatment in certain medical situations but only expresses their general will.
- Decision of the Federal Court of Justice from July 6, 2016 (Az. XII ZB 61/16): In this case, the Federal Court of Justice decided that an advance directive is only valid if it contains specific instructions for dealing with particular medical situations. A mere general rejection of life-sustaining measures is therefore insufficient.
- § 1901a BGB: This provision of the Civil Code regulates the requirements for the effectiveness of advance directives. It states, among other things, that an advance directive must be in writing and signed by the author in their own handwriting.
- Decision of the Higher Regional Court Hamm from September 27, 2011 (Az. I-8 W 72/11): The Higher Regional Court Hamm ruled that an advance directive is invalid if it is not clearly formulated enough to provide the treating physicians with unambiguous instructions for action. In this case, the doctors had carried out a life-sustaining measure despite the patient having rejected such a measure in her directive. However, the court found that the directive was poorly formulated and thus had no binding effect.
Recommendations from Associations and Organizations
Various associations and organizations recommend that patients review their advance directives every few years to ensure that they still reflect their wishes. Changes in the medical field and legislation may also necessitate an update of an advance directive.
For instance, the church office of the EKD (Evangelical Church in Germany) addresses this concerning Christian advance directives.
A review should also occur if there is a change in one’s health status, such as a new diagnosis or a deterioration in health.
It is also recommended that the advance directive be regularly discussed with family members and medical professionals to ensure that it is understood and that the patient's wishes can be taken into account in an emergency.
Organizations such as the German Hospice and Palliative Foundation, the German Society for Palliative Medicine, and the German Foundation for Patient Protection also recommend that an advance directive be used in combination with a power of attorney.
A power of attorney allows one person to authorize another to make decisions on their behalf when they are no longer able to do so. Together with an advance directive, a power of attorney can help ensure that the patient's wishes are implemented in an emergency, even if unforeseen circumstances arise.
Further Articles
- Overview of Costs: What does an advance directive cost?
- In Case of Emergency Without a Directive: Who decides if there is no advance directive?
- For Printing: Advance directive to print.
- Advance Directive Explained Simply: What is an advance directive?